MET is a gene that encodes a receptor tyrosine kinase that is activated upon binding with hepatocyte growth factor (HGF, or Scatter Factor). Specifically, MET is a Continue reading
Category Archives: Oncogenes
Anti-APRIL Antibody BION-1301 for Multiple Myeloma
Multiple myeloma (MM) is a cancer of plasma cells in the bone marrow. Plasma cells are B lymphocytes (B-cells) that have been activated to produce immunoglobulins. When plasma cells become cancerous, the produce copious amounts of immunoglobulins and proliferate in the bone marrow, causing crowding-out of other essential hematopoietic cells, leading to reduced numbers of functioning white blood cells (leukopenia leading to immunosuppression), red blood cells (anemia), and megakaryocytes (thrombocytopenia). Continue reading
ALK-positive lung cancer – antibodies to fusion protein
Approximately 7% of patients with non-small cell lung cancer (NSCLC) possess a transgene that results from an inversion of chromosome 2 that juxtaposes the 5’ end of the echinoderm microtubule-associated protein-like 4 (EML4) gene with the 3′ end of the anaplastic lymphoma kinase (ALK) gene, resulting in the novel fusion oncogene EML4-ALK . Continue reading
Blocking Protein-Protein Interactions in Cancer
The last twenty years has been an unprecedented time in biology – in sequencing the genome and studying the functions of proteins, as well as in unraveling signal transduction pathways, the fundamental biology of normal and diseased cells has been elucidated to a great extent. Although many druggable targets have been identified, it has largely been impossible to target protein-protein interactions (PPI) in drug development. In fact, only ONE drug that targets a PPI has been approved. Continue reading
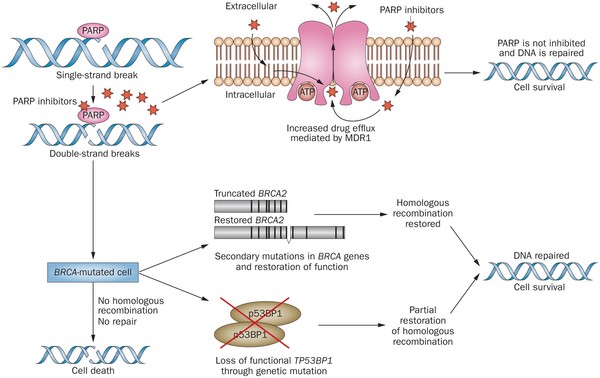
Olaparib – PARP inhibitor for triple negative breast cancer
Olaparib (Lynparza) is a PARP (poly-ADP ribose polymerase) inhibitor that was approved by the FDA in 2014 for the treatment of patients with advanced ovarian cancer who have mutated BRCA1,2 gene. Recently, the drug showed a 70% reduction in risk of progression in patients with less-advanced disease in the maintenance therapy setting:
The Phase III SOLO-2 trial demonstrated a significant improvement in progression-free survival (PFS) in germline BRCA-mutated (gBRCA), platinum-sensitive, relapsed ovarian cancer patients treated with Lynparza (olaparib) tablets (300mg twice daily) compared with placebo in the maintenance setting. The trial met its primary endpoint of investigator assessed PFS (HR 0.30; 95% CI 0.22 to 0.41; P<0.0001; median 19.1 months vs 5.5 months).
PARP inhibitors act in a counter-intuitive manner – by blocking PARP in the context of mutated BRCA1, the cell becomes overwhelmed with double strand breaks, leading to crisis and cell death. BRCA1 mutations, alone, predispose the cell to the accumulation of mutations in protooncogenes and tumor suppressor genes – a few double strand breaks are tumorigenic, whereas a massive number of double strand breaks, as occurs in the context of PARP inhibition, leads to apoptosis.
The use of PARP inhibitors for breast cancer makes great sense, However, in a Phase 3 trial of velparib, an experimental PARP inhibitor, failed to achieve better rates of complete pathogenic response in patients with triple negative breast cancer (TNBC – lack of HER-2, estrogen, and progesterone receptor up-regulation) versus chemotherapy, alone.
At the ASCO conference last week, AstraZeneca presented data on the use of olaparib in 302 patients with BRCA1,2 mutated breast cancer from its OlympiAD trial that compares olaparib against physician’s choice of chemotherapy (capecitabine 2500 mg/m2 d1-14 q 21, or vinorelbine 30 mg/m2 d1,8 q 21, or eribulin 1.4 mg/m2 d1,8 q 21):
OlympiAD Inclusion Criteria:
- Germline mutation in BRCA1 or BRCA2 that is predicted to be deleterious or suspected deleterious.
- Histologically or cytologically confirmed breast cancer with evidence of metastatic disease.
- Prior therapy with an anthracycline and a taxane in either an adjuvant or metastatic setting.
- Prior platinum allowed as long as no breast cancer progression occurred on treatment or if given in adjuvant/neoadjuvant setting at least 12 months from last dose to study entry elapsed.
- ER/PR breast cancer positive patients must have received and progressed on at least one endocrine therapy (adjuvant or metastatic), or have disease that the treating physician believes to be inappropriate for endocrine therapy.
- ECOG performance status 0-1.
- Adequate bone marrow, kidney and liver function.
OlympiAD Exclusion Criteria:
- Prior treatment with PARP inhibitor.
- Patients with HER2 positive disease.
- More than 2 prior lines of chemotherapy for metastatic breast cancer.
- Untreated and/or uncontrolled brain metastases.
Results were quite impressive – this was the first study that demonstrated PARP inhibition is effective in breast cancer:
- About 60% of patients saw their tumors shrink, a hair more than double the 29% objective response rate seen in those patients on chemotherapy.
- Lynparza showed efficacy in patients with TNBC, which is more difficult to treat. AbbVie, which is developing its own PARP inhibitor called veliparib, recentlyannounced a study specifically geared to look at veliparib’s activity in triple negative breast cancer failed to show a benefit when added to chemo.
- Additionally, treatment with Lynparza improved the time to second progression or death compared to chemo,suggesting patients who relapsed after Lynparza experienced a less aggressive return of their cancers.
Astrazeneca is studying olaparib with many combinations, including a study in TNBC with PD-L1 inhibitor durvalumab and CTLA-4 inhibitor tremelimumab.
Regorafenib approved for hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is a primary cancer of the liver that occurs as a result of chronic liver disease, including cirrhosis and hepatitis B and C infections (Figure 1). Serum alpha-fetoprotien (AFP) levels are elevated early in the disease, and screening of patients with chronic liver disease for AFP has lead to earlier diagnosis of HCC. The test is 40-64% sensitive (the ability to detect disease when disease is truly present) because many HCCs do not produce AFP, but it is 75-91% specific (the ability to rule out disease when disease is truly absent) – an AFP of over 400 mg/mL is considered diagnostic. Continue reading
Hyperprogression on Checkpoint Inhibition Immunotherapy
Results with checkpoint inhibitors nivolumab (PD-1, Opdivo), pembrolizumab (PD-1, Keytruda), and atezolizumab (PD-L1, Tecentriq) are impressive. Some patients have experienced incredible and prolonged responses. These drugs are truly modern medical breakthroughs.
Continue reading
NQ01 – a new target for cancer therapy
NQO1 [NAD(P)H:quinone oxidoreductase 1 over-expression has been shown to confer a poor prognosis for patients with cancer of the breast, colon, cervix, lung and pancreas. Recent research indicates that the mechanism involves stabilization HIF-1α (hypoxia inducible factor-1) such that it is not degraded. Continue reading
Tagrisso is superior to platinum-based chemotherapy for patients with relapsed lung cancer following front-line anti EGFR therapy
Tagrisso (osimertinib) is a kinase inhibitor indicated for patients with metastatic epidermal growth factor T790M mutation-positive lung cancer. It was approved under accelerated approval provisions in November 2015 on the basis of phase 2 trials demonstrating a combined overall objective response rate of 59%. Continue reading
Photo-immunotherapy approaches for cancer
The NCI (National Cancer Institute) highlighted two photo-immunotherapy (PIT) approaches that employ antibodies conjugated to phthalocyanine dye IRDye 700DX (IR700). Continue reading