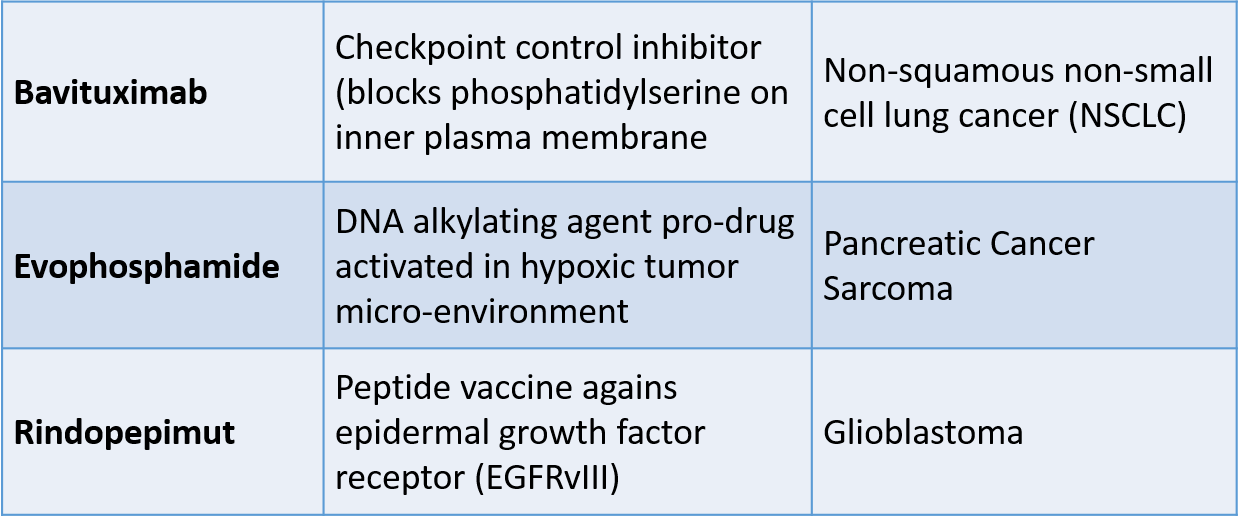
In the last several months, three novel drugs that we have been following on this blog failed in late stage clinical trials. The drugs have diverse mechanisms of action:
Bavituximab – Peregrine Pharmaceuticals
After analyzing the results in the randomized Phase 3 SUNRISE trial comparing bavituximab and docetaxel, the company announced (on February 25) that it is discontinuing the company’s Phase III SUNRISE trial of bavituximab in patients with previously treated locally advanced or metastatic non-squamous non-small cell lung cancer (NSCLC). The decision to stop the trial was based on the recommendation of the study’s Independent Data Monitoring Committee (IDMC) following a pre-specified interim analysis performed after 33% of targeted overall events (patient deaths) in the study were reached. Results of the analysis demonstrated that the bavituximab plus docetaxel group did not show a sufficient improvement in overall survival as compared to the docetaxel group to warrant continuation of the study.
In a previous randomized Phase 2 trial of patients with non-small cell lung cancer, the addition of Bavituximab to docetaxol chemotherapy showed a trend toward increased overall survival (median 11.7 months versus 7.3 months), progression-free survival, and overall response rate. The SUNRISE trial was based on these results.
Bavituximab is a monoclonal antibody that binds to Phosphatidylserine (PS), a phospholipid normally residing in the inner leaflet of the plasma membrane that becomes exposed on tumor cells. Exposure of PS is enhanced in response to chemotherapy, irradiation and oxidative stresses in the tumor microenvironment. PS exposure in tumors promotes an immunosuppressive microenvironment which includes the recruitment of myeloid derived suppressor cells (MDSCs) and M2-like macrophages. Binding of antibodies PS targeting antibodies on tumors triggers an Fc-FcR mediated pro-inflammatory cytokine response that reactivates the immune system and enhances anti-tumor immunity by blocking the immunosuppressive action of PS.
Evophosphamide (TH-302) – Threshold Pharmaceuticals
In December 2015, the company announced the outcomes of two Phase 3 cancer studies (MAESTRO and TH-CR-406/SARC021) of evofosfamide (previously known as TH-302), an investigational hypoxia-activated prodrug, which is being evaluated for first-line treatment of advanced pancreatic adenocarcinoma and advanced soft tissue sarcoma, in combination with chemotherapy. The Phase 3 studies are being conducted under Threshold’s collaboration with Merck KGaA, Darmstadt, Germany.
In the Phase 3 MAESTRO study, patients with previously untreated, locally advanced unresectable or metastatic pancreatic adenocarcinoma treated with evofosfamide in combination with gemcitabine did not demonstrate a statistically significant improvement in overall survival (OS) compared with gemcitabine plus placebo (hazard ratio [HR]: 0.84; 95% confidence interval [CI]: 0.71 – 1.01; p=0.0589).
In the Phase 3 TH-CR-406/SARC021 study being conducted in collaboration with the Sarcoma Alliance for Research through Collaboration (SARC), patients with locally advanced unresectable or metastatic soft tissue sarcoma treated with evofosfamide in combination with doxorubicin did not demonstrate a statistically significant improvement in OS compared with doxorubicin alone (HR: 1.06; 95% CI: 0.88 – 1.29).
Evophosphamide (a bromo-analog of ifosfamide, a DNA alkylating agent) is, a prodrug that is activated only under hypoxic conditions commonly found in the tumor microenvironment. Within regions of tumor hypoxia, evofosfamide releases bromo isophosphoramide mustard (Br-IPM), a potent DNA alkylating agent. Br-IPM kills tumor cells by forming DNA crosslinks, rendering cells unable to replicate their DNA and divide as well as interfering with the transcription of DNA to make essential proteins. Once activated in hypoxic tissues, Br-IPM can also diffuse into surrounding oxygenated regions of the tumor and kill cells there via a “bystander effect.” Because of its preferential activation in the targeted hypoxic regions of solid tumors, evofosfamide may be less likely to produce broad systemic toxicity seen with untargeted cytotoxic chemotherapies.
Rintega (rindopepimut) – Celldex Pharmaceuticals
On March 7, Celldex announced that the independent Data Safety and Monitoring Board (DSMB) has determined, based on a preplanned interim analysis, that continuation of the Phase 3 ACT IV study of RINTEGA (rindopepimut) in patients with newly diagnosed EGFRvIII-positive glioblastoma will not reach statistical significance for overall survival in patients with minimal residual disease, the primary endpoint of the study, as both the RINTEGA arm and the control arm are performing on par with each other. In the ACT IV study, RINTEGA has performed consistently with prior Phase 2 studies but the control arm has significantly outperformed expectations (Hazard ratio = 0.99; median OS: RINTEGA 20.4 months vs. control 21.1 months).
Celldex had built hopes for the drug around a Phase II study that looked promising for patients with EGFRvIII-positive glioblastoma. Looking at progression-free survival, the drug scored a higher PFS rate than the control arm. But investigators concluded at an interim analysis in the Phase III that the control arm was doing slightly better than the drug arm. Patients in the drug arm achieved a median OS of 20.4 months while the control arm survived 21.1 months.
Rindopepimut (Rintega), is a genetically engineered peptide designed to trigger an immune system response to a specific cancer marker called EGFRvIII. That molecular marker can be seen in up to 30% of patients with glioblastoma. This mutation involves the extracellular binding domain (EGFRvIII) and results in a constitutive firing of the tyrosine kinase residues that activate the Akt/PKB pathway.
Rindopepimut is conjugated to Keyhole Limpet Hemocyanin (an immune adjuvant), which elicits a humoral (antibody) and cell-mediated response. EGFRvIII is tumor-specific epitope expressed on approximately 20%–30% of GBMs, 78% of breast carcinomas, 73% of ovarian carcinomas, 42% of head and neck squamous cell carcinomas, and 39% of non-small-cell lung cancers. EGFRvIII expression typically occurs in the presence of wild-type EGFR overexpression, occurring in 58% to 65% of such cases. As wild-type EGFR overexpression most frequently occurs in primary (de novo) GBM and rarely in secondary GBM (those that progress from low-grade tumors), EGFRvIII expression is most common in primary tumors.
I hope that analysis of the Phase 3 trials will reveal subgroups of patients who benefited from the treatments so that they may be approved by the FDA and become available to patients.