Researches with the Ovarian Tumor Tissue Analyses Consortium analyzed the CD8+ (cytotoxic T-cell) content of tumors from 5,500 patients and compared them with clinical outcome. The analysis was large enough to allow for comparison by histologic subtype – endometrioid, clear cell, mucinous, and low-grade serous ovarian cancer, as well as high-grade serous ovarian cancer. Included in the sample were 3,200 high grade serous ovarian cancers.
The strongest link between the number of TILs and overall survival was for patients with high-grade serous ovarian cancer, which is the most common and most lethal histological type, or histotype, of the disease. For these patients, as the number of TILs in tumors increased there were corresponding improvements in survival.
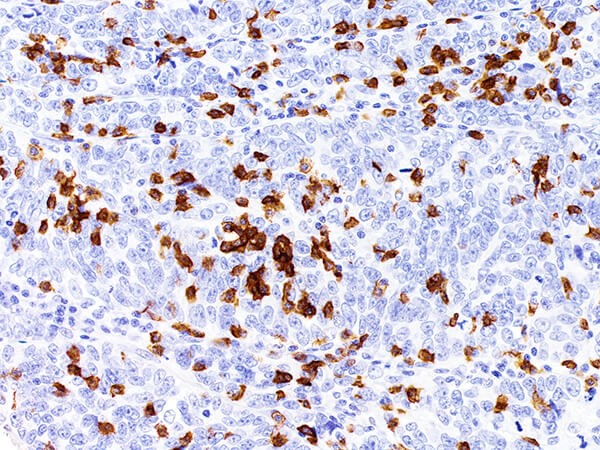
Figure 1. Histological image of a high-grade serous ovarian carcinoma with high levels of CD8+ TILs (brown). https://www.cancer.gov/news-events/cancer-currents-blog/2017/ovarian-cancer-tils-survival
Survival correlated with CD8+ presence – none (2.8 years), low (3 years), moderate (3.8 years), or high (5.1 years). A correlation was seen in patients with high grade serous ovarian cancer who inherited BRCA1 mutations, but not in those with inherited BRCA2 mutations.
Looking at the other histologic types, CD+ positivity was correlated with survival among patients with endometrioid and mucinous tumors, but not for clear cell or low grade serous ovarian cancer.
Clear cell and mucinous cancers were more likely to have no CD8+ positive cells. However, patients with clear cell ovarian cancer respond well to immune checkpoint (anti-PD-1) therapy. This seems counter-intuitive – serous tumors would be considered “cold” tumors, yet, immune checkpoint blockade induces responses in these patients. The authors concluded that more information is needed before clinicians can identify which ovarian cancer patients will respond to checkpoint therapy.
How do these results jibe with the literature?
In a 2003 study of 186 patients with ovarian cancer, researchers found that patients whose tumors contained CD8+ T-cells had much better clinical outcomes:
There were significant differences in the distributions of progression-free survival and overall survival according to the presence or absence of intratumoral T cells (P<0.001 for both comparisons). The five-year overall survival rate was 38.0 percent among patients whose tumors contained T cells and 4.5 percent among patients whose tumors contained no T cells in islets. Significant differences in the distributions of progression-free survival and overall survival according to the presence or absence of intratumoral T cells (P<0.001 for both comparisons) were also seen among 74 patients with a complete clinical response after debulking and platinum-based chemotherapy: the five-year overall survival rate was 73.9 percent among patients whose tumors contained T cells and 11.9 percent among patients whose tumors contained no T cells in islets. The presence of intratumoral T cells independently correlated with delayed recurrence or delayed death in multivariate analysis and was associated with increased expression of interferon-γ, interleukin-2, and lymphocyte-attracting chemokines within the tumor. The absence of intratumoral T cells was associated with increased levels of vascular endothelial growth factor.

Figure 2. Survival Analyses of Patients with Ovarian Carcinoma, According to the Presence or Absence of Intratumoral T Cells. Panels A and B show Kaplan–Meier curves for the duration of progression-free survival and overall survival, respectively, according to the presence or absence of intratumoral T cells in 174 patients with stage III or IV epithelial ovarian cancer and complete, partial, or no response to therapy. Panels C and D show Kaplan–Meier curves for the duration of progression-free survival and overall survival, respectively, according to the presence or absence of intratumoral T cells in 74 patients with stage III or IV epithelial ovarian cancer and a complete response to therapy. Panels E and F show survival curves stratified according to the extent of residual disease for the 74 patients with a complete response to therapy, according to the presence or absence of intratumoral T cells. Optimal debulking was defined by residual tumor of less than 1 cm, and suboptimal debulking by residual tumor of 1 cm or more. P values were derived with the use of the log-rank statistic. http://www.nejm.org/doi/full/10.1056/NEJMoa020177#t=articleTop
In 2005, another group of researchers also saw a correlation between the presence of tumor-infiltrating CD8+ T-cells and clinical outcome in a series of 117 patients. However, it was the ratio of CD8+ to FOXP3+ cells (CTL’s/Treg’s) that was most important:
The median follow-up of the patients was 31 months. Patients with higher frequencies of intraepithelial CD8+ T cells demonstrated improved survival compared with patients with lower frequencies [median = 55 versus 26 months; hazard ratio = 0.33; confidence interval (C.I.) = 0.18–0.60; P = 0.0003]. However, the subgroups with high versus low intraepithelial CD8+/CD4+ TIL ratios had median survival of 74 and 25 months, respectively (hazard ratio = 0.30; C.I. = 0.16–0.55; P = 0.0001). These results indicate that CD4+ TILs influence the beneficial effects of CD8+ TIL. This unfavorable effect of CD4+ T cells on prognosis was found to be due to CD25+forkhead box P3 (FOXP3)+ regulatory T cells (Treg; suppressor T cells), as indicated by survival of patients with high versus low CD8+/Treg ratios (median = 58 versus 23 months; hazard ratio = 0.31; C.I. = 0.17–0.58; P = 0.0002). We conclude that intraepithelial CD8+ TILs and a high CD8+/Treg ratio are associated with favorable prognosis in epithelial ovarian cancer.
Can CD8+ tumor infiltrating T-cells be increased?
In an effort to augment the efficacy of checkpoint inhibitors, researchers are attempting to turn “cold tumors” – those with no CD8+ T cells – “hot” by employing many different intratumoral strategies including chemotherapy, radiotherapy, IL-12, TLR-9, and others. One such approach is currently ongoing – Celsion is evaluating intraperitoneal GEN-1, a liposomal plasmid containing the IL-12 gene. In the Ovation Study, GEN-1 was administered in a neo-adjuvant setting with front-line carboplatin and paclitaxel:
The GEN‐1 + T/C treatment resulted in significant increases in IFN‐γ levels and decreases in VEGF levels in peritoneal fluid. Immunohistochemical analysis of tumor tissue for various T‐cell population showed reduction in immunosuppressive T‐cell phenotype in several patients. The ratio of cytotoxic CD8+ T cells to immunosuppressive FoxP3, IDO1 and PD‐1 expressing cells was also increased in a majority of patients.

Thymosin alpha 1 is a proven upregulator of CD8s