Entinostat is currently in a Phase III trial in combination with Aromasin (exemestane – aromatase inhibitor that blocks the synthesis of estrogen) in patients with metastatic breast cancer who have recurred following treatment with an aromatase inhibitor.
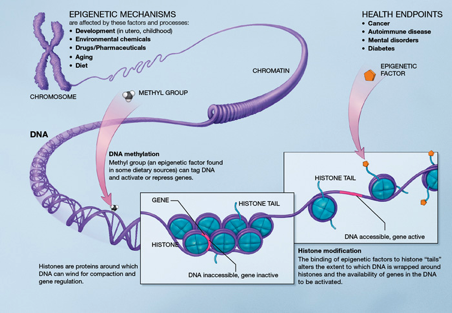
Entinostat is an HDAC (histone de-acetylase) inhibitor – by blocking the removal of acetyl groups from histones, entinostat keeps chromatin in a more transcriptionally active state. One of the mechanisms of resistance to aromatase inhibitors is the down-regulation of estrogen receptors expression via epigenetic regulation. Entinostat reverses this and restores aromatase sensitivity to cancer cells that have become resistant to aromatase inhibitors by virtue of loss of expression of ER:
ERα and aromatase upregulation resulted in sensitization of breast cancer cells to estrogen and letrozole (an aromatase inhibitor). Tumor growth rate was significantly lower in tumor xenografts following treatment with ENT alone and in combination with letrozole than in control tumors (P > 0.001). ENT plus letrozole also prevented lung colonization and growth of tumor cells, with a significant reduction (P > 0.03) in both visible and microscopic foci. Our results show that ENT treatment can be used to restore the letrozole responsiveness of ER-negative tumors. More generally, they provide a strong rationale for immediate clinical evaluation of combinations of histone deacetylase and aromatase inhibitors to treat ER-negative and endocrine-resistant breast cancer.
But, entinostat does more than simply affect epigenetic regulation – it disrupts other cancer pathways, including Her/2, MAPK, and Akt/PKB:
The growth rates of tumors of mice treated with the combination of entinostat with letrozole or exemestane were significantly slower than with the single agent (P < 0.05). Analysis of the letrozole-resistant tumors showed entinostat increased ERα expression and aromatase activity but downregulated Her-2, p-Her-2, p-MAPK, and p-Akt. However, the mechanism of action of entinostat in reversing acquired resistance did not involve epigenetic silencing but rather included posttranslational as well as transcriptional modulation of Her-2. Entinostat treatment reduced the association of the Her-2 protein with HSP-90, possibly by reducing the stability of Her-2 protein. In addition, entinostat also reduced Her-2 mRNA levels and its stability. Our results suggest that the HDAC inhibitor may reverse letrozole resistance in cells and tumors by modulating Her-2 expression and activity.
Because of the activity entinostat has shown on these cancer pathways, a Phase I study of etinostat in combination with Tykerb (lapatinib – HER-1 and HER-2 tyrosine kinase inhibitor) and Herceptin (trastuzumab) is underway in patients who have recurred following treatment with Herceptin.
Last July, researchers at Johns Hopkins published results showing that entinostat in combination with checkpoint inhibitors (CTLA4 and PD-1), showed enhance efficacy (80% cure rate) in mouse models. Checkpoint inhibitors, which block the abrogation phase of the immune response against cancers, are active only if the host is capable of mounting an immune reaction in the first place. It appears that entinostat may affect the immune avoidance mechanisms that protect cancer cells, particularly myeloid-derived suppressor cells (MDSC’s).
These results prompted Merck to enter into a collaboration with Syndax to combine entinostat with Keytruda (PS-1 inhibitor) in Phase Ib/II trials in melanoma and non-small cell lung cancer.