Today’s post is a response by Dr. Bryan Pilkington to Dr. Stan Terlecky’s July 15, 2019 Terlecky’s Corner post entitled, “When is a Brain Really Dead?” Dr. Pilkington is an Associate Professor at Seton Hall University.
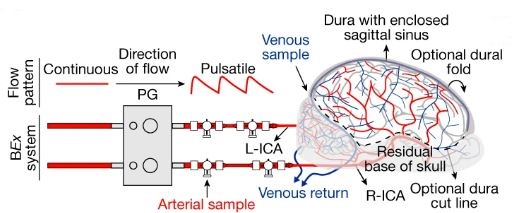
Last month’s Terlecky’s Corner post raises the question, “When is a brain really dead?” The reanimation – to borrow Terlecky’s phrase and his caution about its use – of porcine brains is both exciting and concerning. The excitement is due, as Terlecky notes well, to the possible benefits of such work: “potentially impacting several health scourges of our time including Alzheimer’s disease, Parkinson’s disease, and other age-related neurodegenerative disorders.”[1] He also notices that ethicists will be busy sorting through these and future studies, especially if the human brain gets involved.

This is how the usual dialectic goes when addressing ethical questions about emerging medical technologies. Undoubtedly, there will be lectures and papers from ethicists raising the usual kinds of questions, many titled with some version of, “We can, but should we?” These are not endeavors without merit; ethical analysis often lags behind research; in many cases, something has to be created in order to have something about which to raise questions. In fact, one of the important tasks of ethicists in this realm is to serve as watchdogs: to give caution, to aid researchers in thinking through possible concerns, and in some instances – at least with respect to IRB oversight – to say “no.”[2] However, though this is a useful and important role, it comes at a cost. Many times, those raising these kinds of concerns are termed “the ethics police”[3] and this image has hurt collaboration on research and made more challenging the necessary interprofessional tasks that medical research and healthcare practices are.
So what should be said in response to this kind of research? What are the answers to Terlecky’s list of ethical questions? The questions require longer answers than the space of a blog post admits, but I’ll take a shot at two sets of questions, suggesting a model for answering them and those remaining.
The first set comprises a list of real and immediate questions about one of the practical consequences of this research: organ donation. Will donation rates plummet? Will the organ shortage increase because there will be hold outs who think reanimation is possible? Will public trust diminish as this research moves forward?[4] Will families request that additional healthcare resources be spent on loved ones who meet the legal definition of brain death? An answer which avoids the problematic policing approach but takes seriously the importance of these questions is to engage in an extended conversation with researchers, ethicists, healthcare practitioners and administrators, and members of their communities about new technology, how it might be used, and its far-reaching implications. We must not shy away from these hard questions nor from recognizing the potential value of certain kinds of research, but we must also keep in mind the possible negative externalities that could result. This approach raises more questions. Should this research be halted if it damages public trust? Should it be stopped if fewer organs are donated? These questions lead to further questions. If the organ shortage is a primary concern, is it appropriate to connect it to this research? The conversation I am suggesting must consider that, as well. Some have argued that the sale of organs should be allowed and that this would alleviate the shortage[5], others have raised concerns about the commodification of human beings if such sale is legalized[6] – the breadth of the needed conversation is wide, as answers to questions about organ sale are connected to ethical concerns raised about porcine brain experimentation.
A second set of questions hover around the definition of death and the sources upon which we rely to answer those questions. Terlecky helpfully asks about the legal, ethical, and spiritual determinations of death. From where or in what do we root our conceptions of life, of human flourishing, and of death? Are they religious? Are they legalistic? Are they rooted in metaphysical conceptions of the person that we learned in our undergraduate philosophy courses? The kind of conversation I am suggesting is most effectively held when we bring the deep and rich traditions that inform our thought to bear on the subject matter under discussion. It is not a simple task to work through various traditions and try to understand how others think about reanimated porcine brains, human brains, and death, but that is what is needed. As physician and ethicist Lauris Kaldjian recently asked of his colleagues,[7] did you take a course about the existential questions in medical school? Though rhetorical, the suggestion is powerful. How should we respond to this research? In the same way we should respond to all research that raises significant ethical questions, by practically reasoning together.
References:
[1] Terlecky, S. 2019, July 15. “When is a Brain Really Dead?”
[2] Evans, J. 2012. The History and Future of Bioethics: A Sociological Account. Oxford, United Kingdom: Oxford University Press.
[3] Klitzman, R. 2015. The Ethics Police? The Struggle to Make Human Research Safe. Oxford: Oxford University Press
[4] Moschella, M. 2018. Brain death and organ donation: A crisis of public trust. Christian Bioethics 24(2):133–50.
[5] Cherry, M. 2005. Kidney for Sale by Owner: Human Organs, Transplantation, and the Market. Georgetown University Press.
[6] Pilkington, B. 2018. A Market in Human Flesh: Ramsey’s Argument on Organ Sale, 50 years later. Christian Bioethics 24(2):133–50.
[7] Kaldjian, L. (Personal communication during lecture in Grand Rapids, Michigan, March 25, 2019).
 To reconnect as a community during the COVID-19 pandemic, SHU University Libraries seek your stories of what this time has been like for you. We hope that sharing these stories with one another will bring us back together in a new way, through sharing our personal experiences of this moment.
To reconnect as a community during the COVID-19 pandemic, SHU University Libraries seek your stories of what this time has been like for you. We hope that sharing these stories with one another will bring us back together in a new way, through sharing our personal experiences of this moment.



 By
By