Somewhat lost in the worldwide COVID-19 health crisis is the continued destruction of lives through opioid abuse. Metaphorically speaking, it is as if the COVID-19 tsunami landed on a beach already flooded by the storm of the opioid abuse epidemic. One crisis does not mitigate the effects of the other; indeed, early data point to increasing opioid use, with already unacceptable consequences only looking to get worse.
Perhaps COVID-19’s effects on substance abuse was predictable – the pandemic has impacted people in numerous ways, many independent of actual viral infection. Social distancing requirements result in increased isolation and alienation. Economic turmoil has caused widespread unemployment (or reduced employment), leading many people to experience deep financial stress and anxiety. For those battling past abusive/addictive behaviors, the pandemic is a relapse catalyst – setting in motion a return to highly destructive actions, attitudes, and decisions. Opportunities to speak with healthcare professionals, therapists, faith-based counselors, or other support personnel are severely curtailed. These conditions facilitate the surge in opioid use and abuse being witnessed across the nation.

What could possibly be done when two such health crises collide? We can only begin to attempt an answer here:
First, we must remove the stigma associated with opioid abuse. It should be recognized that opioid and related substance abuse/addiction represents a disease state – involving biological, environmental, and behavioral factors. It is not about moral failings, but neural networks; less about poor decision making, and more about limited perceived options. Individuals experiencing addiction deserve respect and an understanding of the toll of dependency; to marginalize them is demeaning and counterproductive.
COVID-19-related social distancing mandates lead to a reduction of diversions available to potential opioid users/abusers. Fewer people are around to witness and help prevent or treat potential overdoses.
In healthcare, there is an emergent consensus on the effectiveness of medication-assisted treatment (MAT), defined by the Substance Abuse and Mental Health Services Administration (a division of the U.S. Department of Health and Human Services) as “the use of FDA-approved medications, in combination with counseling and behavioral therapies, to provide a “whole-patient” approach to the treatment of substance use disorders.”[1] MAT is not replacing one drug with another – this would be an incomplete understanding of the therapy program. The use of buprenorphine, methadone and naltrexone, in combination with counseling and social support/behavioral interventions, have dramatically altered the landscape of opioid use disorder treatment. MAT works – and works well. The problem is the limited number of physicians trained and licensed to administer MAT. Physicians must receive a Drug Addiction Act of 2000 (DATA) waiver (also known as an “X” waiver) to prescribe the requisite drugs and deliver the appropriate behavioral therapies. Physicians may become waivered after 8 hours of didactic training; medical students require 8 hours of specialized training coupled with a clinical experience demonstrating MAT’s use with opioid use disorder patients. Only a small percentage (<10%) of practicing physicians in this country possess the waiver; of those, less than half actually deliver MAT. Some 40% of counties in the U.S. do not have a waivered physician. Tens of thousands of citizens die from opioid use disorder every year – we must increase the number of X waivered physicians and encourage more to practice the therapy.
If there is any silver lining to the COVID-19 crisis, it is the enabling of telemedicine. For those sheltering in place but requiring access to the health system, telemedicine offers a world of new possibilities. Every attempt must be made to promote digital literacy in vulnerable populations to maximize the impact of this technology.
Recognizing the devastation wrought by COVID-19’s impact on opioid abuse disorders, several local and state jurisdictions across the country are trying to help. As per recommendations made by the American Medical Association[2],[3], several changes are afoot. Buprenorphine may now be prescribed to patients by phone or telemedicine encounter. Methadone is being prescribed in amounts that will last almost a month. These lifesaving drugs are being delivered directly to patients in their homes. The process to have prescriptions refilled has also been streamlined – for example, no toxicology or other testing is required. These developments enable care without the risk of exposure to COVID-19 inherent in in-person visits. Finally, naloxone is being recognized as the true overdose wonder drug – and is being far more liberally distributed.
These are incredibly difficult times – with a global viral-based pandemic intersecting with a devastating substance abuse epidemic. However, as with all crises, good ideas, critical reasoning, and evidence-based decision making will chart a course for real change and true improvement. It cannot happen too quickly for all those affected by opioid use disorders.
SRT – July 2020
References:
[1] Medication-Assisted Treatment (MAT). (2020, April 30). Retrieved July 06, 2020, from https://www.samhsa.gov/medication-assisted-treatment
[2] COVID-19 policy recommendations for OUD, pain, harm reduction. (2020, July 2). Retrieved July 06, 2020, from https://www.ama-assn.org/delivering-care/public-health/covid-19-policy-recommendations-oud-pain-harm-reduction
[3] Taking action on opioid use disorder, pain & harm reduction during COVID-19. (2020, July 2). Retrieved July 06, 2020, from https://www.ama-assn.org/delivering-care/opioids/taking-action-opioid-use-disorder-pain-harm-reduction-during-covid-19

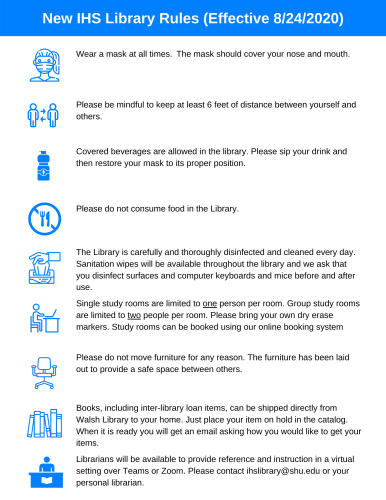
 The IHS Library recently introduced “Workshop Wednesdays,” a weekly instructional session series that meets Wednesdays at 12pm over Zoom. Workshops range from an
The IHS Library recently introduced “Workshop Wednesdays,” a weekly instructional session series that meets Wednesdays at 12pm over Zoom. Workshops range from an