


Operationalizing the Right to Health through the Pandemic Influenza Preparedness Framework
by Mark Eccleston-Turner Developing states lack access to pandemic influenza vaccines. The provision of ‘essential’ medicines is a core, non-derogable obligation of the right to health in the International Covenant on Economic, Social and Cultural Rights (ICESCR),...Global Health Governance: The Role of Feedback
Blog by Sara Gorman, PhD, is an MPH candidate at Columbia University Mailman School of Public Health photo credit: Logo of the World Health Organization via photopin There is a lot of talk about global health governance these days, especially in the wake of the Ebola...Institutional Readiness in Practice of Pandemic Response to an Emerging Infectious Disease
Asif B. Farooq and Shannon E. Majowicz This paper argues that emerging and re-emerging infectious diseases (EIDs) remain a threat-focused security issue as the relative success of recent international responses do not fully reflect our current readiness for EID...
The Rise of A Deadly New Strain of Bird Flu: Has China Handled This Properly So Far?
Yanzhong Huang, Editor Senior Fellow for Global Health, Council on Foreign Relations This is a cross-post with CFR’s Asia Unbound Blog. China has long been perceived as the epicenter of major infectious disease outbreaks. The 2003 SARS crisis was the most recent...
Ten Years after SARS: Five Myths to Unravel
Ten Years after SARS: Five Myths to Unravel Yanzhong Huang, Editor Senior Fellow for Global Health, Council on Foreign Relations This is a cross-post with CFR’s Asia Unbound Blog. Last week, I was in Beijing for an international conference while the...
Sustainability of Sub-Regional Disease Surveillance Networks
Sustainability of Sub-Regional Disease Surveillance Networks Melinda Moore, David J. Dausey, Bounlay Phommasack, Sok Touch, Lu Guoping, Soe Lwin Nyein, Kumnuan Ungchusak, Nguyen Dang Vung, and Moe Ko Oo Sub-regional disease surveillance networks are an emerging trend...
The WHO Meeting on Controversial H5N1 Research: What Happened, and What Does It Mean?- David Fidler
The WHO Meeting on Controversial H5N1 Research: What Happened, and What Does It Mean? David P. Fidler, GHG Contributing Blogger James Louis Calamaras Professor of Law, Indiana University Maurer School of Law The conclusion of the much anticipated meeting at the World...
The WHO Meeting on Controversial H5N1 Research – David Fidler
The WHO Meeting on Controversial H5N1 Research: What Implications for Global Health Governance? David P. Fidler, Contributing GHG Blogger James Louis Calamaras Professor of Law, Indiana University Maurer School of Law The World Health Organization (WHO) is hosting a...Multilevel Governance and Complex Threats: The Case of Pandemic Preparedness in the European Union and the United States
Multilevel Governance and Complex Threats: The Case of Pandemic Preparedness in the European Union and the United States Erik Brattberg and Mark Rhinard The scale of dangers...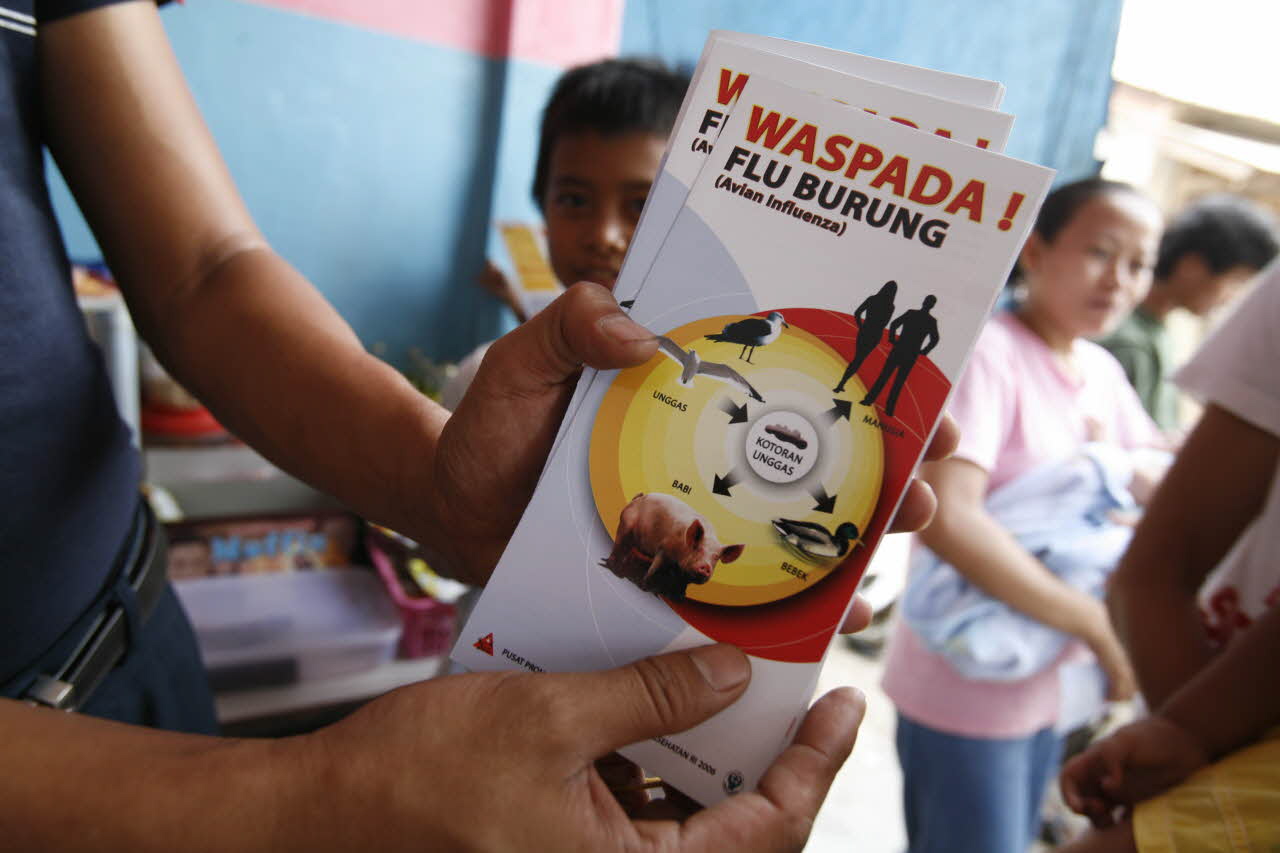
Epidemics as Politics with Case Studies from Malaysia, Thailand, and Vietnam
Epidemics as Politics with Case Studies from Malaysia, Thailand, and Vietnam Tuong Vu Severe epidemics caused by severe acute respiratory syndrome (SARS) and avian influenza viruses have recently killed hundreds of people while causing chaos and panic in many...
H1N1 – The Social Costs of Cultural Confusion
In May 2011, the World Health Assembly received the report of its International Health Regulations Review Committee examining responses to the outbreak of the 2009 H1N1 pandemic influenza and identifying lessons to be learnt. This will emphasized the need for better risk communication in the future. But risk and communication are not objective facts; they are socially mediated cultural products. Responses to crises are not simply determined by the situation at hand, but also mental models developed over protracted periods. Accordingly, those forces responsible for promoting the precautionary approach and encouraging the securitization of health, that both helped encourage a catastrophist outlook in this instance, are unlikely to be held to scrutiny. These cultural confusions have come at an enormous cost to society.
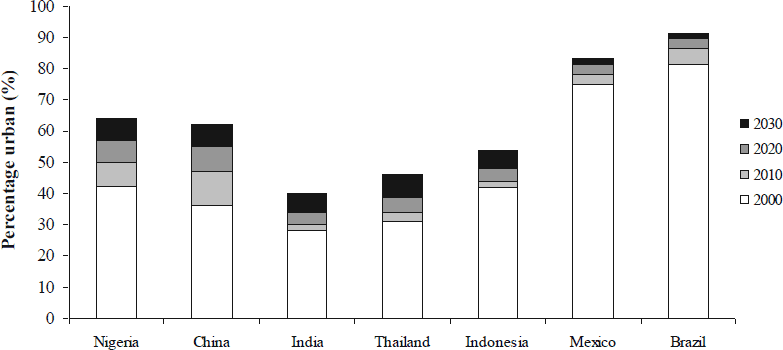
The International Flow of Risk: The Governance of Health in an Urbanizing World
In 2008, the world’s urban population exceeded its rural population for the first time. The United Nations estimates that about 15% of the world’s population now lives in “megacities” of 10 million or more people, or in near-megacities of 5-10 million. Three-quarters of the megacities are in low- and middle-income nations, where rural-to-urban migration will drive rapid urbanization through 2050. Services and infrastructure rarely keep pace with population growth. Even in well-resourced cities, municipal leaders struggle with urban sprawl, unmet housing and transportation needs, environmental degradation, and disaster vulnerabilities. In the absence of adequate resources and regulation, informal settlements and markets evolve fluidly, creating shelter and livelihoods but also exposing inhabitants to environmental risks that exacerbate health inequities. These problems might once have been considered local challenges. Now, these “international cities” are often cross-roads for the movement of people, animals, and goods (and the health risks that they carry), as well as drivers of national or regional economic development. New strategies are needed to govern the flow of health risks within and among these densely populated urban centers. The breathtaking scope of the challenges that urbanization poses for development and security can only be understood by looking at long wave events that cross sectors, disciplines, and borders. Tools such as the Framework Convention on Tobacco Control and the International Health Regulations (2005) can affect the flow of health risks between regions, but cannot substitute for strong planning, policy, and management functions at the municipal level – exactly where governance capacities tend to be weakest.

Global Health Security: Closing the Gaps in Responding to Infectious Disease Emergencies
Rising concerns about the human, political, and economic costs of emerging infectious disease threats and deliberate epidemics have highlighted the important connection between global public health and security. This realization has led security communities, particularly in the U.S., to seek ways to bolster the international health response to public health emergencies as a means of protecting national security. While there have been important recent efforts to strengthen international response to infectious disease threats, there are areas that deserve more attention from both the health and security communities. In this article, we describe two important gaps in international frameworks that govern the response to global public health threats which can negatively affect the security of states: (1) despite attempts to strengthen international rules for responding to public health emergencies, there continues to be strong disincentives for states to report disease outbreaks; and (2) systems for detecting and responding to outbreaks of infectious diseases are hindered by a lack of standards of practice for sharing biological samples and specimens. To address these gaps in global governance of infectious disease threats, additional incentives are needed for states to report disease outbreaks to the international community; there should be greater enforcement of countries’ international health obligations; and both political and scientific communities should develop workable practice standards for sharing biological samples of all types.

Mandatory Influenza Vaccinations: An Example of Health Promotion Theater
Mandatory Influenza Vaccinations: An Example of Health Promotion Theater Anita Miko and Monica K. Miller In 2009, New York became the first state to issue a policy requiring health care personnel to obtain influenza vaccinations. This law can be described as “health...
