To date, the search for biomarkers to best guide active immunologic therapy selection and monitoring of response has not been fruitful. Unlike molecular targeted therapies and monoclonal antibodies for which the presence of mutated or over-expressed proteins (e.g., Philadelphia Chromosome, B-raf, HER-2, and CD20) is a prerequisite to use, no such biomarkers have been identified for active immunotherapies, for example Provenge (autologous dendritic cell therapy for prostate cancer), Yervoy (ipilimumab), and Keytruda (PD-1 inhibitor for melanoma).
AstraZeneca/MedImmune seeks to change this with its acquisition of Definiens, a company that combines sophisticated and automated image analysis of cancer tissue specimens (e.g., immunohistology, tissue microarrays, fluorescent in situ hybridization) and molecular data mining to provide quantitative analyses that identify important biomarkers for personalized treatments.
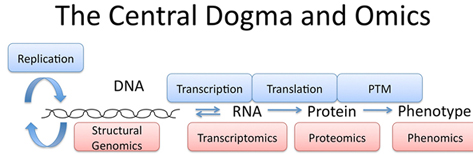
The technology is called Phenomics. It has to do with examining the phenotype of tissues using many different analytical tools.
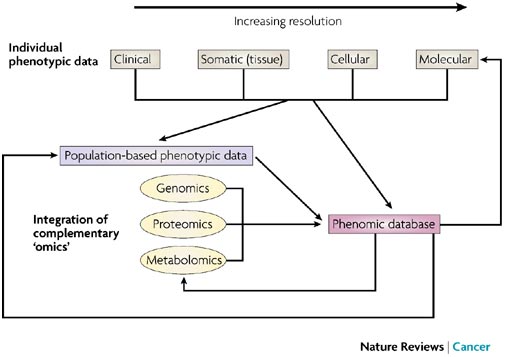
The phenome has been defined as the complete phenotypic representation of the species, and phenomics defined as the study of variation in the phenotype that results from the combined influence of genetic and environmental variation. Central to the success of phenomics is the collection of quantitative phenotypic traits, often at the molecular or cellular level. Phenomic tools continue to mature. These include imaging technology, from conventional radiograms to imaging at the cellular and sub-cellular levels. Additionally, electronic medical records are becoming widely used, and will enable the seamless and automated transfer of data to phenotype databases.
Definiens is working on an Immunoscore as a predictive and prognostic marker for patients with melanoma who are treated with ipilimumab (Yervoy).
Using the Immunoscore to evaluate outcomes after primary surgery for rectal cancer, Definiens found that:
the densities of CD3(+) and CD8(+) lymphocytes and the associated Immunoscore (from 10 to 14) were significantly correlated with differences in disease-free and overall survival (HR, 1.81 and 1.72, respectively; all P < 0.005). Cox multivariate analysis supports the advantage of the Immunoscore compared with the tumor-node-metastasis (TNM) staging in predicting recurrence and survival (all P < 0.001). Lymph node ratio added information in a prognostic model (all P < 0.05). In addition, high infiltration of CD3(+) and CD8(+) lymphocytes in tumor biopsies was associated with downstaging of the tumor after pCRT (CD3(+) cells; Fisher exact test P = 0.01)