CARMA Therapeutics, a company that develops chimeric antigen receptor technology, not for T-cells (CAR-T cells), rather, for macrophages, hence the name “CARMA,” closed on an initial round of funding to advance its technologies. Continue reading
Category Archives: Immunology & Immunotherapy
Olaparib – PARP inhibitor for triple negative breast cancer
Olaparib (Lynparza) is a PARP (poly-ADP ribose polymerase) inhibitor that was approved by the FDA in 2014 for the treatment of patients with advanced ovarian cancer who have mutated BRCA1,2 gene. Recently, the drug showed a 70% reduction in risk of progression in patients with less-advanced disease in the maintenance therapy setting:
The Phase III SOLO-2 trial demonstrated a significant improvement in progression-free survival (PFS) in germline BRCA-mutated (gBRCA), platinum-sensitive, relapsed ovarian cancer patients treated with Lynparza (olaparib) tablets (300mg twice daily) compared with placebo in the maintenance setting. The trial met its primary endpoint of investigator assessed PFS (HR 0.30; 95% CI 0.22 to 0.41; P<0.0001; median 19.1 months vs 5.5 months).
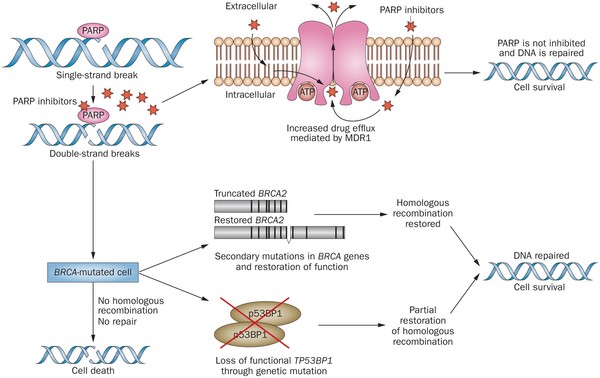
PARP inhibitors act in a counter-intuitive manner – by blocking PARP in the context of mutated BRCA1, the cell becomes overwhelmed with double strand breaks, leading to crisis and cell death. BRCA1 mutations, alone, predispose the cell to the accumulation of mutations in protooncogenes and tumor suppressor genes – a few double strand breaks are tumorigenic, whereas a massive number of double strand breaks, as occurs in the context of PARP inhibition, leads to apoptosis.
The use of PARP inhibitors for breast cancer makes great sense, However, in a Phase 3 trial of velparib, an experimental PARP inhibitor, failed to achieve better rates of complete pathogenic response in patients with triple negative breast cancer (TNBC – lack of HER-2, estrogen, and progesterone receptor up-regulation) versus chemotherapy, alone.
At the ASCO conference last week, AstraZeneca presented data on the use of olaparib in 302 patients with BRCA1,2 mutated breast cancer from its OlympiAD trial that compares olaparib against physician’s choice of chemotherapy (capecitabine 2500 mg/m2 d1-14 q 21, or vinorelbine 30 mg/m2 d1,8 q 21, or eribulin 1.4 mg/m2 d1,8 q 21):
OlympiAD Inclusion Criteria:
- Germline mutation in BRCA1 or BRCA2 that is predicted to be deleterious or suspected deleterious.
- Histologically or cytologically confirmed breast cancer with evidence of metastatic disease.
- Prior therapy with an anthracycline and a taxane in either an adjuvant or metastatic setting.
- Prior platinum allowed as long as no breast cancer progression occurred on treatment or if given in adjuvant/neoadjuvant setting at least 12 months from last dose to study entry elapsed.
- ER/PR breast cancer positive patients must have received and progressed on at least one endocrine therapy (adjuvant or metastatic), or have disease that the treating physician believes to be inappropriate for endocrine therapy.
- ECOG performance status 0-1.
- Adequate bone marrow, kidney and liver function.
OlympiAD Exclusion Criteria:
- Prior treatment with PARP inhibitor.
- Patients with HER2 positive disease.
- More than 2 prior lines of chemotherapy for metastatic breast cancer.
- Untreated and/or uncontrolled brain metastases.
Results were quite impressive – this was the first study that demonstrated PARP inhibition is effective in breast cancer:
- About 60% of patients saw their tumors shrink, a hair more than double the 29% objective response rate seen in those patients on chemotherapy.
- Lynparza showed efficacy in patients with TNBC, which is more difficult to treat. AbbVie, which is developing its own PARP inhibitor called veliparib, recentlyannounced a study specifically geared to look at veliparib’s activity in triple negative breast cancer failed to show a benefit when added to chemo.
- Additionally, treatment with Lynparza improved the time to second progression or death compared to chemo,suggesting patients who relapsed after Lynparza experienced a less aggressive return of their cancers.
Astrazeneca is studying olaparib with many combinations, including a study in TNBC with PD-L1 inhibitor durvalumab and CTLA-4 inhibitor tremelimumab.
Imfinzi, the latest approved checkpoint, and checkpoint combinations
The latest checkpoint inhibitor to be approved is AstraZeneca’s Imfinzi (durvalumab), a monoclonal antibody directed against PD-L1, which is expressed on cancer cells.
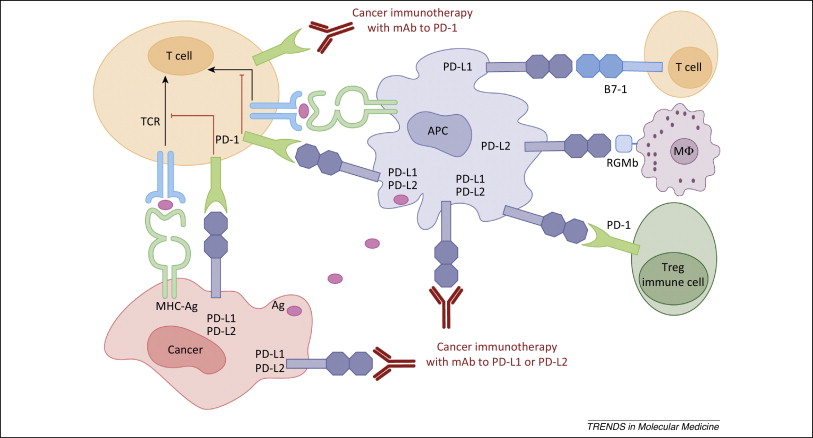
Figure 1. PD-1 / PD-L1 axis. http://www.cell.com/trends/molecular-medicine/references/S1471-4914(14)00183-X
TIGIT, a CTLA4-esque Immune Checkpoint for Cancer
Immune checkpoint-directed therapy is producing unprecedented clinical results in many patients. So much so, that the FDA recently reversed its longstanding policy or approving cancer drugs based on site of origin, to the presence of a biomarker (microsatellite instability (MSI-H) or mismatch-deficient repair (dMDR) as the indication for therapy with pembrolizumab (Ketruda), and PD-1 blocker. Cancers expressing MSI-H or dMDR mutate at a rapid rate, presenting novel epitopes to the immune system, which is readily mobilized against them so that tumor infiltrating T-cells are reliably present. Blocking the PD-1/PD-L1 pathway in this context allows for prolongation of the immune response and better clinical results. Continue reading
Platelet conjugates effectively deliver checkpoint inhibitors to tumors
Platelets are the second most abundant cellular component of blood. The platelet membrane contains an abundance of receptors to facilitate interactions with subendothelial matrix , other blood cells, and other platelets. The central role of platelets is in hemostasis, however, they also contain copious amounts of cytokines that induce inflammation. Continue reading
PD-L1 Inhibitor, avelumab, approved for Merkel cell carcinoma
Avelumab (Bavencio) is a PD-L1 inhibitor that was approved for the treatment of patients with metastatic Merkel cell carcinoma (MCC). Continue reading
Hyperprogression on Checkpoint Inhibition Immunotherapy
Results with checkpoint inhibitors nivolumab (PD-1, Opdivo), pembrolizumab (PD-1, Keytruda), and atezolizumab (PD-L1, Tecentriq) are impressive. Some patients have experienced incredible and prolonged responses. These drugs are truly modern medical breakthroughs.
Continue reading
Ublituximab, a novel anti-CD20 Monoclonal Antibody for CLL
TG Therapeutics is developing ublituximab, and anti-CD20 monoclonal antibody for patients with CLL (Chronic Lymphocytic Leukemia). In a phase 3 study in patients with relapsed disease, the combination of ublituximab and ibrutinib (Imbruvica) was superior to ibrutinib, alone – the overall response rates were 80% and 47%, respectively. Continue reading
Juno Advances CAR T-cell CAR017 and Halts CAR015 in Non-Hodgkin Lymphoma
Juno Therapeutics is developing Chimeric Antigen Receptor (CAR) T-cells directed against B-cell antigen CD19 for the treatment of patients with B-cell lymphomas. The company has elected to halt the development of JCAR015 for Acute Lymphoblastic Leukemia (ALL) and proceed with JCAR017 for relapsed/refractory diffuse large B-cell lymphoma (DLBCL), the most common form of Non-Hodgkin Lymphoma (NHL), due to the development of cerebral edema and subsequent death of several patients with ALL enrolled in its phase 2 ROCKET trial, which has been suspended. Continue reading
Argos’ Phase 3 Metastatic Renal Cell Carcinoma Study Discontinued by Data Monitoring Committee
Rocapuldencel-T is an autologous dendritic cell immunotherapy for patients with metastatic renal cell carcinoma about which we have written previously. It is produced by isolating patient tumor mRNA, which is then electroporated into patient dendritic cells in the presence of CD40 ligand. The rationale of this approach is to bypass mechanisms by which cancer cells dampen the anti-tumor immune response, including down-regulation of MHC Class I molecules. If the cancer antigens are presented on licensed dendritic cells, logically, the immune system would be appropriately stimulated to attack the cancer. Continue reading